Abstract
Introduction: An increasing number of medical therapies has improved the outcomes of patients with immune thrombocytopenia (ITP), yet a small percentage fail to respond even to multiple medications. While splenectomy can be effective for such refractory cases, it is a less attractive option given its associated surgical morbidity and infectious complications. Partial splenic embolization (PSE) has been proposed as a less invasive and potentially less immunosuppressive procedure which could raise the platelet (Plt) count even after multiple medical therapies have failed. Herein, we aim to report the efficacy of PSE in a contemporary cases series at 2 large academic centers.
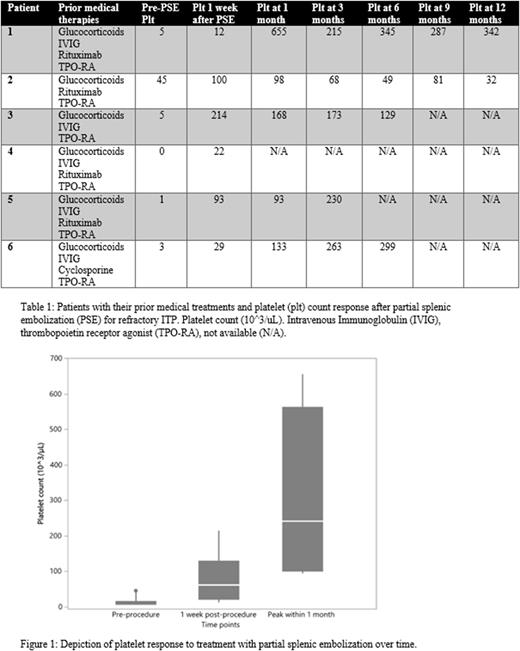
Methods: We retrospectively identified adult patients who had undergone PSE for refractory ITP between March 2018 and Dec 2021. Demographics, comorbid conditions, and prior medical therapies for ITP were obtained from direct chart review. Clinical workup was reviewed to confirm the diagnosis of refractory ITP including elevated immature platelet fraction (IPF), negative disseminated intravascular coagulopathy (DIC) labs, and negative viral studies. Plt count at baseline, prior to procedure and following PSE were recorded at 1 week, 1 month, 3 months, 6 months, 9 months, and 12 months. A partial response (PR) was defined as Plt increase > 30,000/µL and a complete response (CR) was defined as a Plt increase > 100,000/µL following PSE.
Results: A total of 6 patients were identified (median age 62, range 23-69, all patients were males, 5 white and 1 Hispanic). All patients were admitted for management of thrombocytopenia at the time of PSE. 5/6 had presented or developed bleeding complications, with 3/6 having mild symptoms (petechiae, hematoma, epistaxis), 2/6 gastrointestinal bleeding, and no intracranial bleeding. No patients required rapid increase in Plt for an urgent procedure. PSE was pursued in 2 patients with cirrhosis as a comorbidity, which was thought to be contributing to splenomegaly and thrombocytopenia. Despite cirrhosis, a separate diagnosis of ITP was documented due to acute drop in plt count and additional clinical work-up. Median Plt count prior to PSE was 4,000 (interquartile range [IQR] 2-15, range 1-45). All patients had received glucocorticoids and at least one thrombopoietin receptor agonist, 5/6 had received intravenous immunoglobulin (IVIG), 4/6 had received rituximab and 1/6 had also received cyclosporine. At 1 week following PSE, 1/6 had achieved a PR and 2/6 had achieved CRs for an overall response rate (ORR) of 50%. Plt continued to increase in all subjects within a month, and CRs were achieved in 5/6 patients and a PR in the remaining subject (Table 1 & Figure 1). The ORR at 1 month was 100% and the median peak Plt was 242,000/µL (range 93-655). Primary adverse events following PSE were mild and included either abdominal pain or diarrhea in all patients.
Conclusions: Overall, PSE for management of ITP is rarely utilized in clinical practice. Our small case series highlights the overall effectiveness of this procedure in refractory cases. This series demonstrates PSE as a safe and effective method of treating ITP in cases refractory to medical management.
Disclosures
Kis:Bela Kis: Consultancy; Siemens: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal